
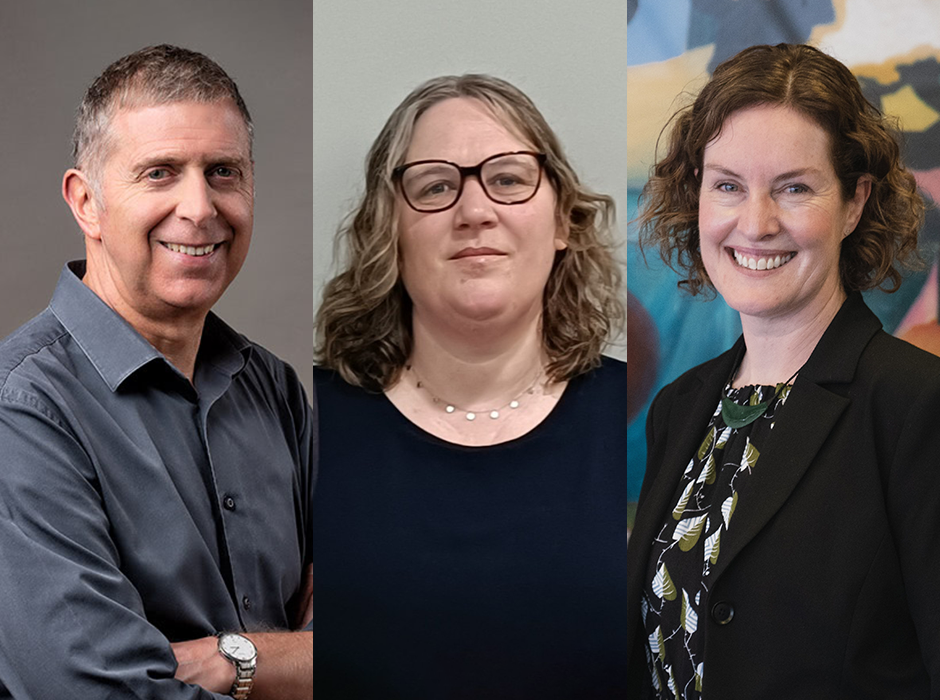
From left, Dr Sarah McKenzie, Professor Ben Wheeler and Dr Paula O'Kane.
The demand for recently-funded diabetes technology is likely to skyrocket by up to 400 per cent in coming years, but the public health system is not equipped to meet this need, an Otago researcher says.
Professor Ben Wheeler, from the Department of Women and Children’s Health at the University of Otago – Ōtākou Whakaihu Waka, has been awarded almost $1.4 million to develop a new model of care for faster and more equitable access to automated insulin delivery (AID) for people with type 1 diabetes.
Professor Wheeler is one of 12 Otago researchers to receive funding in the latest Health Research Council funding round, totalling more than $4.6 million.
Type 1 diabetes affects up to 25,000 people in Aotearoa New Zealand, with loss of up to 20 years life expectancy reported, especially in those diagnosed at a young age, and of Māori/Pacific ethnicity.
Approximately 15-20 per cent of people with type 1 diabetes are currently using AID, Professor Wheeler says.
Pharmac-funded access to the “gold standard” AID technology was widened in late 2024, which will see demand for AID use by people with type 1 diabetes increase to 70 – 80 per cent in the coming years – an increase of up to 400 per cent, he says.
“Unfortunately, with this widened access the public health system is not meeting the demand, and many are missing out or experiencing large waiting lists to access training and systems.
“Some regions have even suspended training due to health workforce challenges.”
Only between 500 to 1000 people with type 1 diabetes are currently able to be trained to use the technology annually out of 12,000 – 15,000 people who are expected to seek AID, he says.
“This is creating massive inequity based on ethnicity, location (rural vs urban), and socio-economic status.”
Professor Wheeler’s research seeks to provide a solution by evaluating a model of AID training and remote support developed in Otago’s world-leading AID research trials.
It also removes post-code lotteries to access by providing fly-in-fly out training throughout NZ, and remote support regardless of home region/post-code.
“We hope to demonstrate that our proposed model of care can be scaled up and lead to fast, effective, safe and equitable access to advanced diabetes technology throughout New Zealand.
“Without this funding we would be unable to undertake this research – particularly research so directly connected to improving diabetes care throughout all of New Zealand.”
Dr Sarah McKenzie, from the Department of Psychological Medicine, University of Otago, Wellington, is “extremely grateful” to have received an HRC Career Development Award of more than $170,000 to explore the unique challenges men face accessing mental health support via primary care.
Men are often less likely than women to seek help for mental health difficulties, but very little is known in New Zealand about the specific challenges men face accessing support, Dr McKenzie says.
“That means mental distress often goes undetected or untreated among men.
“This is significant considering three-quarters of all suicides in New Zealand occur among men, with over half having contact with primary healthcare services in the six months leading up to their death.”
Her research will be conducted in collaboration with colleagues in primary healthcare, to better understand men’s experiences of accessing mental health support as well as the difficulties healthcare professionals encounter in delivering services to men.
Dr Paula O’Kane, from the Department of Management, received a grant of almost $30,000 to undertake a pilot study in Dunedin to understand what older adults in Aotearoa value when ‘ageing in place’.
Existing research indicates that ageing in place has different meanings and connotations within different communities and this could include ageing in your own home, or valuing the importance of community, she says.
“Understanding what our local communities in Dunedin (and eventually beyond) need and want to age successfully is vital to the wellbeing of older people.”
Receiving the HRC funding means researchers involved in the Collaboration of Ageing Research Excellence Otago Research Theme can begin the potentially impactful project that will hopefully be expanded nationally and with key universities globally, she says.
Nine Otago researchers were also awarded funding from the New Zealand Lottery Grants Board, totalling more than $1.1 million.

Associate Professor Benjamin Darlow (left) and Associate Professor Hamish Jamieson.
Grants
Health Research Council Health Delivery Research Project Grant
Professor Benjamin Wheeler, Women's & Children's Health, $1,399,996
Diabetes technology - New model of care for faster and more equitable access
Advanced diabetes technology and automated insulin delivery is now clearly the gold standard for type 1 diabetes care in New Zealand and worldwide. However, the majority of people with diabetes, particularly adults have yet to access this care due to a variety of reasons. Pharmac will soon allow unrestricted funding to these systems, but current models of care are unable to cope with the expected demand, a shift from 10-15 per cent use currently to 70-80 per cent use over the coming years (as seen overseas). In addition, if this shift follows current patterns, the increase will largely first occur in those who are European, with already in-target diabetes, with less deprivation, and those living in urban settings. The aim is to shift the model of care to allow first, fast, safe, and equitable access to those who need it the most - those out-of-target with a focus on priority populations.
Associate Professor Benjamin Darlow, Primary Health Care and General Practice (UOW), $1,399,989
Enhancing Non-operative Care Of ACL Rupture: Equity and Effectiveness (ENCORE)
Anterior cruciate ligament (ACL) rupture is a serious knee injury that affects thousands of New Zealanders annually with long-term impacts on pain, function, work, and sports. ACL rupture is managed with rehabilitation or surgery. Most people should complete rehabilitation before considering surgery, but most New Zealanders receive surgery as first-line care. Two years following ACL surgery, one-third of people have ongoing unacceptable symptoms and almost half have osteoarthritis. This is worse for Māori and people from Pacific communities. New evidence suggests ACL ruptures can heal without surgery and the novel Cross-Bracing Protocol may increase healing. The Enhancing Non-operative Care Of Rupture: Equity and Effectiveness (ENCORE) trial will compare the Cross-Bracing Protocol to rehabilitation alone, measuring pain, symptoms, sports, work, quality of life, costs, ligament healing, and need for surgery.
Associate Professor Hamish Jamieson, Medicine (UOC), $1,399,974
Virtual cognitive stimulation therapy - an online treatment for dementia mate wareware
This study examines the effectiveness of virtually delivered cognitive stimulation therapy for individuals with mild to moderate dementia (mate wareware) and assesses both the impact and cost-effectiveness of the intervention and gather user feedback. The study commences with qualitative investigations into the context of delivering a virtual intervention in Aotearoa New Zealand followed by a pragmatic randomised controlled trial (pRCT). Outcomes focus on cognition, quality of life, and communication outcomes, supplemented by qualitative assessments of user experiences and an economic analysis of pRCT data. Emphasising a Māori-centred, tikanga-based approach in settings involving Māori, the project aims to use telehealth to address access barriers, particularly for those in rural areas or with mobility constraints addressing ethnic and geographic diversity in health service access and aiming to provide post-diagnosis support for people living with dementia (mate wareware). The project is underpinned by longstanding working relationships with the dementia community to ensure impact.
From left, Professor Warwick Duncan, Dr Andrea Clark and Professor Suetonia Green.
Health Research Council Health Delivery Research Career Development Award
Dr Sarah McKenzie, Psychological Medicine (UOW), $170,565
Improving men’s access to mental health support via primary care
Health Research Council Health Delivery Research Activation Grant
Dr Fiona Imlach, Public Health (UOW), $30,000
Economic cost of migraine in Aotearoa New Zealand
Dr Nicholas Green, Chemistry, $29,015
Identifying next generation therapeutics for colorectal cancer
Professor Suetonia Green, Dunedin School of Medicine, $29,832
INCH-HD: Incremental dialysis to improve wellbeing and service delivery
Dr Snita Ahir-Knight, Psychological Medicine (UOW) , $30,000
Children of parents with a mental illness: Ethical considerations
Professor Warwick Duncan, Oral Sciences, $29,911
New diagnostic aid for oral cancer screening - an ultrasound elastography device
Dr Paula O'Kane, Management, $29,768
Ageing in place in Ōtepoti, Dunedin
Dr Meredith Peddie, Human Nutrition, $29,652
Messages around physical activity and sitting. Can we do better?
Dr Andrea Clark, Management, $30,000
Co-designing, co-commissioning with and for mental health services

From left, Dr Meredith Peddie, Dr Snita Ahir-Knight and Dr Fiona Imlach.
New Zealand Lottery Grants Board
Professor Ben Wheeler, Women's & Children's Health, $119,957
Closing the loop - Full automated insulin delivery and patch pumps in adults with diabetes
Professor David McBride, Preventive & Social Medicine, $54,878
Veterans & Ex-Serving Project Aotearoa (VESPA): Supporting the mental wellbeing of ex-NZDF members as they re-enter civilian life
Neda Nasrollahi, Psychological Medicine, $159,944
Testing a new treatment regime for people with Treatment-Resistant Depression
Mrs Jane Taafaki, Health Sciences Pacific, $159,877
Understanding occupational health and exposures in rural Pacific meatworkers
Professor Patrick Manning, Medicine, $99,080
Salivary microRNAs as biomarkers of diabetic heart disease
Dr Mak Sarwar, Obstetrics & Gynaecology (UOC), $119,980
Molecular test to triage high-grade cervical abnormalities and improve cervical cancer screening
Dr Timothy Prickett, Medicine (UOC), $112,205
Effect of exercise on musclin and cardiac function in heart failure
Associate Professor Hamish Jamieson, Medicine (UOC), $73,872
Improving the understanding of the hip fracture journey for people following discharge from hospital
Dr Sherly Parackal, Centre for International Health, $119,061
Co-designing a culturally appropriate intervention to reduce the risk of heart disease among high-risk South Asians living in Aotearoa New Zealand
Dr Parimala Kanagasabai, Obstetrics, Gynaecology and Women's Health (UOW), $119,726
Working with (abnormal uterine) periods. What are the impacts and costs?
Associate Professor Jacqueline Keenan, Surgery (UOC), $58,362
Microplastics and increased risk of early-stage bowel cancer