What is IPE ?
Interprofessional education (IPE) occurs when:
"learners of two or more health or social care professions engage in [intentionally] learning with, from and about each other to improve collaboration and the quality of care and services."
Centre for Collaborative Health Professional Education (CAIPE 2017)
Interprofessional education (
For example, students engaged in a particular learning activity might all be final year pre-registration students, or they might be a mix of senior pre-registration and new post-registration students learning together.
Characteristics of IPE

For the interprofessional activity to be considered high-quality
- Learning is common across professions.
- Participants compare and contrast their roles.
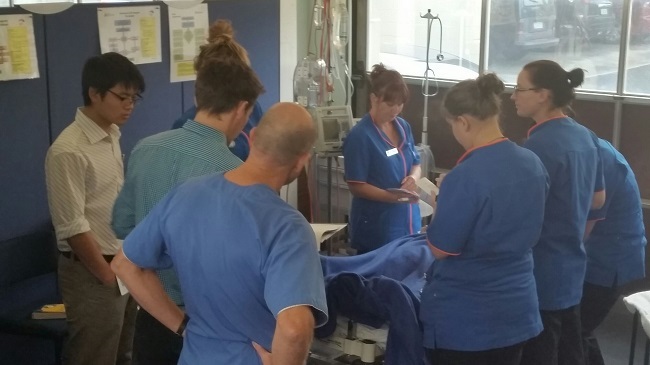
- Learning is interactive.
- Learning optimally involves reflection.
- Activities include experiential learning.
- Planning involves an interprofessional team.
- Learning outcomes include collaboration between professions.
- Activities should challenge stereotypes.
Key to
Learning becomes an exchange among and between learners from different professions that changes how they perceive themselves and others.
In this way,
Why do IPE ?
Ultimately,
The worldwide trend is for health organisations to move from a position of fragmentation to a position of strength. That fragmentation currently comes from working in silos and in isolation – the different professions all approaching the patient/client separately and with a potentially narrow focus. The strength comes from different professions working collaboratively: sharing knowledge and expertise, and approaching the patient/client from a "whole person" focus.
Putting ourselves in the patient's/client's shoes, let's take a look at two examples:
Working in silos
Brian, an 81-year-old man with poor mobility, currently living in an independent villa in a retirement village, is about to be discharged home after a laparoscopic cholecystectomy. On the day of discharge, over a period of five hours, he is seen by the pain team, the surgeon and medical team, the physiotherapist, the nurse, the occupational therapist, and the social worker.
The physiotherapist, nurse, occupational therapist, and social worker all ask him the same or similar questions about how he is going to manage at home, what activities he can do, and the support he is going to need. Once seen by all these people, he is sent to the transit lounge on a different floor, where another nurse brings him his discharge information / medications.
Working collaboratively
Brian, an 81-year-old man with poor mobility, currently living in an independent villa in a retirement village, is about to be discharged home after a laparoscopic cholecystectomy. On the day of discharge he is first seen together by the pain team, surgeon, and nurse. They decide from a post-surgery perspective he is ready to be discharged, however they are aware the family have concerns about how he will manage at home.
They ask for the input of the interdisciplinary team to assess how he will manage at home and ask them to then have a brief meeting with the registrar and nurse to decide a joint discharge management plan. The interdisciplinary team decide the skills of the physiotherapist and social worker are most needed in this situation, but that they will call on the nurse and occupational therapist if needed.
Together the physiotherapist and social worker meet with Brian and a broad physical and social needs assessment is undertaken using completing a common assessment / recording format. Together with the registrar and nurse, they decide on a funded pack of community home support.
By 11am, Brian has been given a copy of the discharge information—including the home support care—and has had the discharge medications and wound care instructions explained by his nurse.
How would IPE have helped in this setting?
- Learning in an interprofessional way would have prepared the staff for working more collaboratively to meet Brian's needs.
- Collectively, the team would be prepared and able to tap into each other's specialist skills, for the benefit of Brian.
- The team would have been communicating more effectively.
- The team would have been working effectively together, towards the common goal of meeting Brian's needs in an efficient way.
Benefits of IPE
With the world moving towards more collaborative practice in healthcare,
IPE helps students to build and establish good collaborative practice through the course of their learning.- Students increase their understanding of the role, skills and perspectives of other professions.
- Students develop and demonstrate an improved respect towards other professional groups due to this increased understanding.
- Students learn how to build interprofessional networks, and their value.
IPE facilitates a shift from passive learning to an active exchange of information, knowledge and understanding that changes how the student perceives themselves and others and their thoughts around professional roles and interactions.- Patients/clients/whānau experience a greater consistency of care due to enhanced collaboration.
- Patients/clients/whānau don't have to repeat the same information multiple times, preventing information from “falling through the gap”.
- Patients/clients/whānau experience a faster progression with their health treatment.
Worldwide drivers
Despite good intentions, health care systems have become increasingly fragmented and inefficient. The World Health Organization describes education for, and implementation of, collaboration as important ways to move health care systems from fragmentation to positions of strength: i.e. to boost the sustainability and efficiency of these systems for high-quality, patient-centred care.
- "The World Health Organization (WHO) and its partners recognise interprofessional collaboration in education and practice as an innovative strategy that will play an important role in mitigating the global health workforce crisis" (Framework for Action on Interprofessional Education & Collaborative Practice, WHO, 2010).
- The world is experiencing a global health worker shortfall, projected by WHO to reach 10 million by 2030, and this is impairing the provision of essential, life-saving interventions.
- There are current financial drivers to do more with less.
- Funding opportunities are becoming increasingly scarce with increased competition as health services vie for the same funding.
National drivers
Nationally, we have health care challenges ahead of us in New Zealand. Many of the Government's health targets relate to the need for improvements in health associated with chronic diseases and for those with the highest health needs. Collaborative practice has been shown to improve these health outcomes, and so students should be prepared for working in a collaborative practice environment.
"To develop the health workforce, we want to encourage greater flexibility to work across professions and boundaries as part of multi-disciplinary teams."
Minister of Health. 2023. New Zealand Health Strategy.